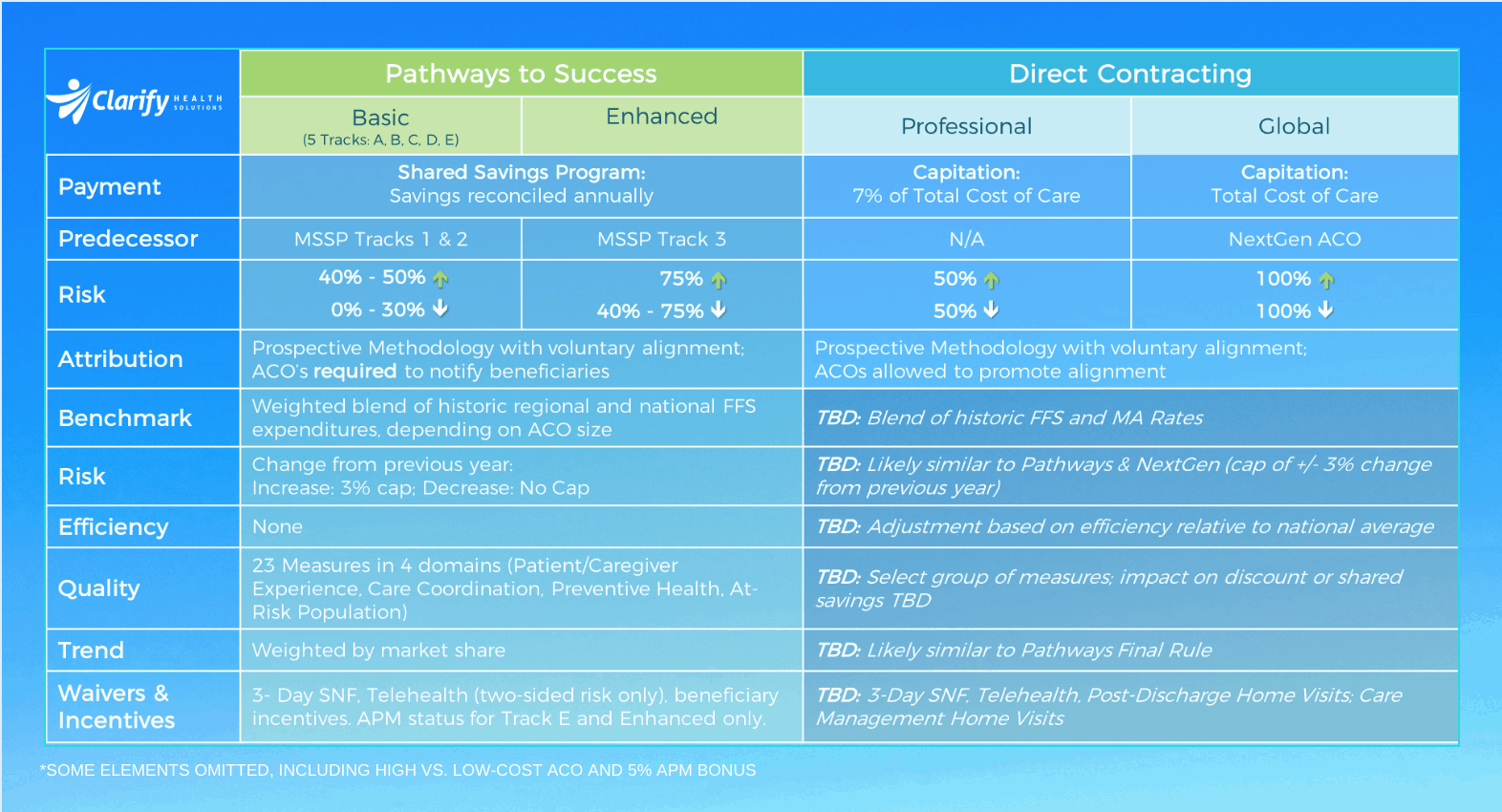
Are you deciding how to best participate in a Medicare ACO? Read our guide for deciding with an edge. In 2017, if Track 1 MSSP ACOs had been operating under the new Pathways to Success rules, 40% of them would have ended the year with losses-owed to CMS. They would have owed up to $270M ($76 avg PMPY) to CMS.1 Conversely, Track 1 ACOs who outperformed their benchmarks enough to earn shared savings collectively earned $685M ($226 PMPY) in shared savings that year.2 These ACOs, along with those who have been in more advanced risk-sharing models with CMS (Track 3 and NextGen) must now decide their paths forward. What decisions will they make today, given that they now have access to a much deeper and more accurate set of information than they did in 2017? The introduction of the new population-based payment models from CMS should raise near-term questions for all Medicare ACOs who want to be successful in 2020 and beyond. Today we will dive into the first of three critical considerations introduced in our previous post: How should I participate in Medicare ACOs? There are six options for Pathways to Success – Tracks A, B, C, D, E, and Enhanced. See the graphic above for a high-level overview and side-by-side comparison of each track. As we all know, the most significant change with Pathways to Success is mandatory downside risk. ACOs will no longer be allowed to enter upside-only gainsharing agreements, forcing them to take some measure of downside risk, and the extent of that risk will increase over time. Of course, ACOs now have unprecedented opportunity to participate in considerable savings or gains, particularly with the new Direct Contracting programs. Although we don’t have the final Direct Contracting rule from CMS yet, we are seeing savvy ACOs already positioning themselves for success. With the expanded set of options and the inevitability of downside risk, ACOs should carefully consider how they can make the best decision possible. Those already exposed to significant upside and downside risk should now be even more vigilant. First, ACOs should consider three key criteria as they decide how to participate. Answers to the above questions ought to be foundational considerations amongst ACOs’ other priorities as they make their decisions. Second, ACOs should get started early. ACOs can’t afford to wait until their performance period starts to think about this. To be successful, they need access to these insights now so they can begin to set up infrastructure, process, and targeted change management well in advance of the program start. Every ACO is unique – their patient populations, the needs of their populations, the composition and history of their provider groups, and the challenges faced by these providers in providing the best care they can for their patients. The resources an ACO has available to dedicate to population health along with appetite for change throughout their organization are make-or-break factors. With all these objective and subjective criteria in play, there can be no one-size-fits-all decision criteria or solution. Further, CMS’ multitude of new payment model options creates perhaps unintended complexity in the scenarios that ACOs could and should consider. However, ACO’s can find clarity. Today, information including risk-adjusted benchmarks, assigned patients, utilization insights, and referral insights are all available to ACOs with n=1 precision. Already, some of our customers here at Clarify have made significant changes in their participation structures with the benefit of these insights. ACOs may not have a crystal ball predicting their future performance, but with the right data – they can get a significant edge. And having the data is only the first step. Stay tuned for our next blog post to learn how you should prepare once you’ve made your decision on how to participate. In the meantime, explore our products for value-based program management and success. This article was originally posted in November 2019 and updated in August 2020.What are the payment models, and how have they changed from previous offerings?
How should I position my ACO for success in this new risk-based savings and payment environment?
Just because an ACO is highly-aligned and progressive doesn’t mean they will succeed in a population-based payment model. For instance, those who have observed closely have seen several ACOs drop out of NextGen after paying millions of dollars in losses to CMS. While there are many reasons for this, one crucial reason is that these entities did not know the answers to the above beforehand, and therefore couldn’t accurately forecast their performance. If these organizations had access to this information before committing, how might they have changed their course, and how might they have fared?What participation options are best for my ACO?
1Based on CMS public use files. Revisions to benchmarking methodology for Pathways not incorporated into these numbers. PMPY numbers based on attributed membership to losing ACOs as a denominator.
2Based on membership to Track 1 ACOs who cleared their minimum savings rate and earned savings.
- Author Details