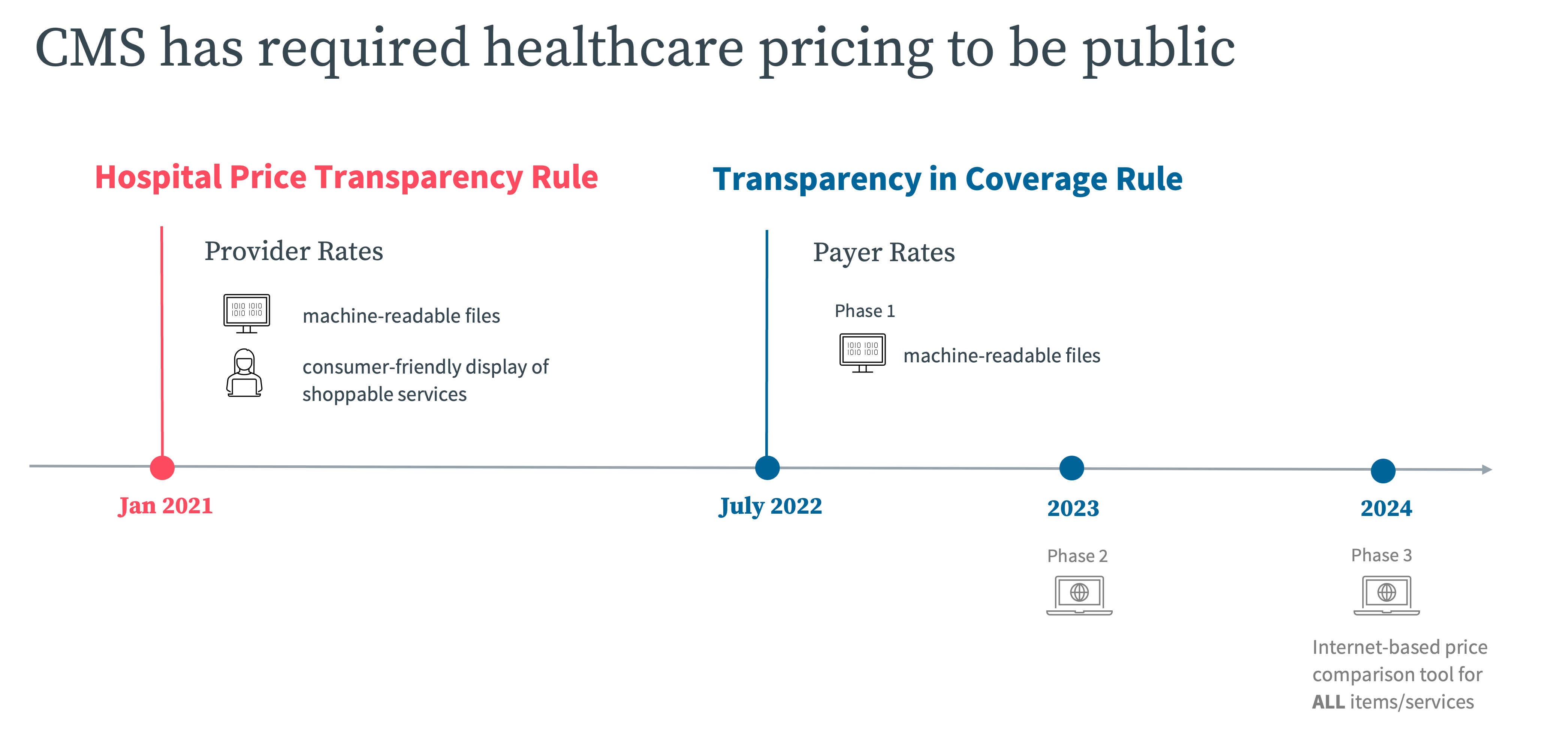
The American healthcare system is ushering in a new era of health cost transparency. After decades of negotiations between health insurance companies and healthcare providers being clothed in secrecy, Americans can now access negotiated prices before receiving care. The Healthcare Price Transparency Act, which came into effect January 1, 2021, requires hospitals to publish their rates in two ways: With U.S. healthcare spending averaging $11,582 per American, minimizing healthcare costs is important. Health cost transparency offers Americans the opportunity to compare hospital rates before taking on large medical bills. Hospitals must publish the rates they negotiate with insurance companies and their cash pay rates – rates they will accept from cash paying patients, which can be lower than health insurance rates. In addition, giving patients visibility into cash pay rates and health insurance rates, hospital rate transparency means patients can shop around between hospitals, comparing prices before their procedures. While comparing rates in the midst of an emergency may be impractical, healthcare price transparency is especially helpful for shoppable services like primary care appointments, x-rays and other imaging, laboratory tests, and routine surgeries. Shopping smart could save a patient thousands of dollars. A 2018 Kaiser Family Foundation study of large employer plans found that allowed in-network charges for joint replacements varied widely between geographical regions, from an average cost as low as $23,170 in Maryland to as high as $58,193 in New York and New Jersey. Whether a patient is due for a routine colonoscopy or searching for the right doctor to perform major surgery, hospital price transparency means patients can take control of their health costs like never before. The Centers for Medicare & Medicaid Services’ Hospital Price Transparency Rule and Transparency in Coverage Rule are now in effect. Here’s the timeline for providers and payers to publicly report on their rates. Niall Brennan, Clarify’s Chief Analytics and Privacy Officer, spoke to Beckers Hospital Review about the rule and said it’s “laudable, but flawed.” The Healthcare Price Transparency Act is only the beginning of sweeping reforms to healthcare price transparency. While hospitals are already required to provide rate transparency, a major health insurer price transparency rule will go into effect on January 1, 2022. Plans will be required to share their negotiated rates for all in-network covered services and items as well as their out-of-network allowed amounts and billed charges. However, CMS won’t enforce this requirement until July 1, 2022. “Until regulations or further guidance is issued, the departments strongly encourage plans and issuers to start working to ensure that they are in a position to be able to begin reporting the required information with respect to 2020 and 2021 data by Dec. 27, 2022,” the guidance from CMS said. As healthcare price transparency grows and patients have the information necessary to choose an affordable provider, providers and hospitals will need to offer competitive rates. As the curtain lifts on negotiated rates, health plans and providers are hoping to enter rate negotiations with better information than ever before. However, hospital rate transparency in its infancy and the unkempt state of rate data available today, many are finding it is not easy feat to make sense of it all. Clarify Rates is a cloud software analytics product that gives providers instant access to the latest market rate data and benchmarks of comparative market performance. It arms your contract negotiations team with the detailed hospital rate intelligence they need to negotiate quickly, effectively, and with confidence. Request a demo of Clarify Rates today.
What’s new for healthcare price transparency in 2021?
Why is price transparency important in healthcare?
Health plan rate transparency is next as reforms continue
Payer-provider rate negotiations are changing
- Author Details





