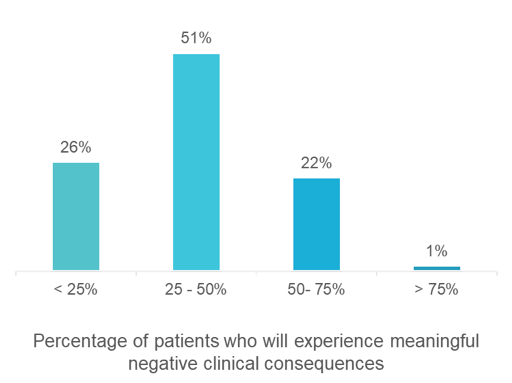
On June 23, 2020, we co-hosted a virtual panel with Bunny Ellerin, President of New York Health Business Leaders (NYCHBL), to interview executives from NewYork-Presbyterian Hospital, CareMount Medical, and Clarify Health about the future of healthcare in New York following the peak of COVID-19. The panel included Emme Deland, Senior Vice President, Strategy, NewYork-Presbyterian Hospital, Richard P. Morel, MD, Chief Physician Executive, CareMount Medical, and Ryan Ahern, MD, Head of Corporate Development, Clarify Health and Clinical Assistant Professor & Attending Physician, Weill Cornell Medical Center. Here is how they responded: Unlikely, the panelists said. However, maybe that is a good thing for our healthcare system. “Anyone who works on the front lines will tell you that some subset of the care is unnecessary,” said Dr. Ahern. However, “the pendulum clearly swung too far,” Ms. Deland said, about the high volume of canceled visits during the peak of the COVID-19 pandemic, but she agreed it might not all return. Many patients are afraid to go to the hospital, clinic, and doctor’s office. During the peak of COVID-19, there were 200 at-home deaths per day, which is ten times the normal amount. While some proportion of these may have been COVID-19 related, the experts attributed a significant number to missed care because of COVID-19 fears. For patients who do go back to receive care in-person, institutions are taking precautions. They are limiting capacity, at least for the time being. They are strategically scheduling appointments to avoid overcrowding in hallways and waiting rooms. They are spacing out the time between visits, especially when clinically necessary. For example, the exam rooms for colonoscopies and endoscopies must be left idle for 20 minutes in case of aerosolization. Even if we can overcome these challenges, the question remains as to whether all patients need the care they deferred or whether it is unnecessary. Of course, it is nuanced—for CareMount, care was more likely to be deferred for gastroenterology, dermatology, ophthalmology, and orthopedics, and less likely for oncology, internal medicine, and cardiology. There are some cases where deferred care is problematic, but other cases where it is not. In a recent survey published by the Kaiser Family Foundation (KFF), which was conducted on May 13-18, 2020, about half of the public said they had skipped or postponed medical care due to the coronavirus outbreak. Of those who delayed their care, 11% said their medical condition worsened. We polled our audience, which was comprised of more than 150 attendees from health plans, health systems, ACOs, provider groups, life sciences companies, technology companies, and other healthcare organizations, on the same topic. We asked them: 51% of the audience said that between 25 and 50% of patients would experience a meaningful negative clinical consequence. According to the KFF survey, nearly 7 in 10 of those who had skipped seeing a medical professional expected to get care in the next three months. Medical professionals across the country are urging patients to seek care if they need it. Here are the ways the NYC healthcare system is making it safer for patients to get the care they need: First, remote care, specifically, telehealth, is being implemented. Prior to COVID-19, NewYork-Presbyterian Hospital had one of the largest telehealth programs in the country, and during COVID-19, they spiked up to 90K telehealth visits per month, for consultations and remote monitoring. “We need to leverage telehealth to keep people out of the hospital,” said Ms. Deland. Telehealth has taken off at CareMount as well. They went from only a handful of visits per day to over 1,500 per day, and that number is now stabilizing at approximately 600 per day. They now have providers who do one day per week of telehealth visits instead of in-person. One of the reasons that telehealth lacked traction prior to COVID-19 was that insurers were concerned that it led to increased costs. With the momentum of COVID-19, “more happened with telehealth in 10 days than 10 years,” said Bunny. Of course, some conditions fare better with telehealth than others. For example, conducting medical reconciliation via telehealth is effective, especially for patients who might otherwise forget to bring their medications into the doctor’s office. It also has a unique place for homebound patients. It can also be an effective tool to see which patients need to be seen right away versus which ones can really wait. It will be an interesting case study to look at the telehealth visit data and determine its impact on outcomes and whether it leads to a reduced cost of care. Can a telehealth visit replace an in-person visit? It is on health systems and providers to demonstrate that to payers. Second, we need to make patients feel more comfortable about getting in-person care. This involves better and more frequent communications, contact tracing, and patient and staff safety (i.e., hand washing and masks). There are also measures being taken to limit the amount of contact per patient. These include e-check-ins or letting patients wait in their car instead of the waiting room, cohort diagnostic testing whereby imaging, diagnostics, and labs are taken at the same visit, and revisiting the fact that New York state has more rooms with double beds than single beds. The panelists predict that there will be future upticks in NYC, likely in the fall when school starts and in December, but this time the city will be prepared, and it will not be the epicenter. NYC hospital executives have learned tough lessons from the crisis about how to prepare for the next peak. Flexibility is critical. During the height of the crisis, NYP more than doubled ICU capacity. Going forward, they need flexibility to be able to quickly flex ICU capacity up and down. They already keep 20% of their beds free for when the next surge happens. They are also focused on refashioning the workforce, determining how and where hospital staff works. They are changing the supply chain inventory approach from “just in time” to “just in case of a pandemic,” as Ms. Deland put it. Lastly, they need cross training to have more flexibility in staffing between the ICU, med-surg, and ED. During the peak of the COVID-19 pandemic, NYC health systems and provider groups under a fee-for-service model were hemorrhaging revenues because of decreased volume. The long-term revenue impact could be severe if volume does not fully rebound. Now, more than ever, systems need to have a clear line of sight into what is driving volume in- and out-of-network. Clarify Referrals, a healthcare analytics software, can help. It prioritizes physicians for engagement and affiliation using the industry’s most precise referral logic and complete dataset. If you want to increase market share and in-network referrals, visit the Clarify Referrals webpage to request a demo. You can watch the full discussion here.
Will patient volume return to pre-COVID-19 levels?
Of the patients who had their care deferred due to COVID-19, what proportion do you expect will experience meaningful negative clinical consequences?
How can we make it safe for patients to come back?
Will there be a resurgence of COVID-19 cases? What are your predictions?
How can we prepare for less patient volume than expected?
- Author Details





